DO NOT USE - ALL INFORMATION LIKELY INCORRECT IF NOT ACTIVELY DANGEROUS
Please use current guidelines available on the UHNM intranet for patient treatment
Please use current guidelines available on the UHNM intranet for patient treatment
'Door-to-needle time' should not exceed 1 hr
- Interval between patient's arrival and commencement of lumbar puncture (if indicated) and antimicrobial treatment ('door-to-needle time') should not exceed 1hr
- If bacterial meningitis strongly suspected, contact a consultant in infectious diseases
RECOGNITION AND ASSESSMENT
Symptoms and signs
- Headache, neck stiffness, photophobia
- Fever
- Impaired consciousness, coma and fits
- Clinical features of septicaemia or severe sepsis
In the elderly, confusion can occur as the only symptom of meningitis in the absence of meningism or even of fever
Life-threatening features
- Altered consciousness
- Focal neurological deficit
- Raised intracranial pressure
- Convulsions
- Concurrent evidence of sepsis
Differential diagnosis
- Subarachnoid haemorrhage
- Other intracranial sepsis
- Systemic sepsis
- Other causes of confusion or of raised intracranial pressure
- Encephalitis
- look for symptoms of confusion, seizures, dysphasia or reduced conscious level
- Malaria in travellers
INITIAL MANAGEMENT
Penicillin allergy
- True penicillin allergy is rare
- Ask the patient and record what happened when they were given penicillin
- If any doubt about whether patient is truly allergic to penicillin, seek advice from a microbiologist or consultant in infectious diseases
Only accept penicillin allergy as genuine hypersensitivity if convincing history of either rash within 72 hr of dose or anaphylactic reaction
Infection control alerts
- Check for IC alert
- if IC alert not available, check previous 12 months of microbiology reports
- If MRSA present, treat as tagged for MRSA. See MRSA management
- If ESBL, MGNB, CARB present, treat as tagged for ESBL. See ESBL/MGNB/CARB management
Immediate management
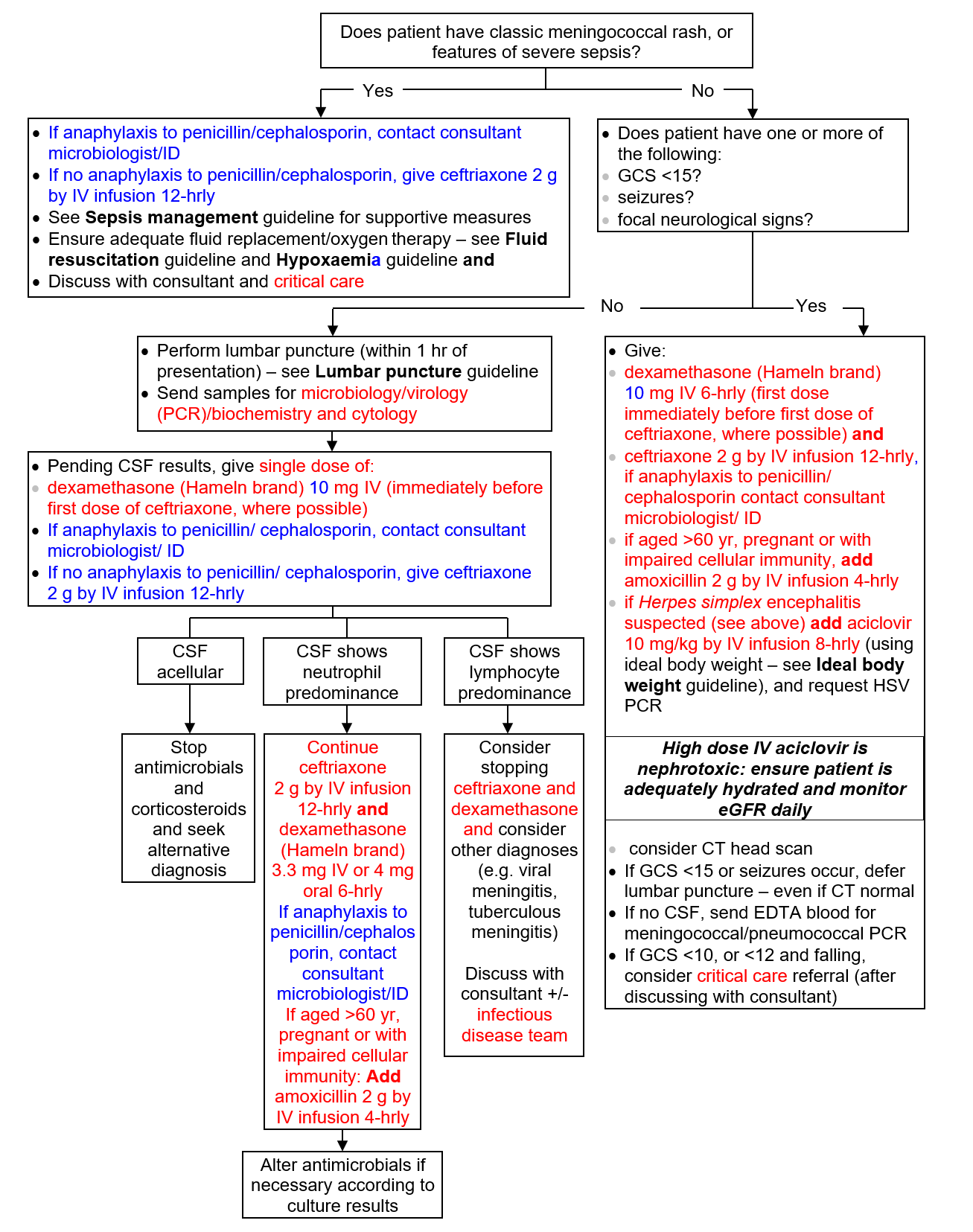
Investigations
- CSF
- if no clinical contraindications, perform lumbar puncture immediately. See Lumbar Puncture guideline
- if no clinical contraindications to LP, CT scan is not indicated
- FBC, differential WBC and coagulation screen
- U&E, glucose and CRP
- Chest X-ray
Microbiology
- Throat swab (Include suspected meningococcal meningitis in clinical details. Take separate swabs for MRSA screening)
- Blood culture
- Meningococcal/pneumococcal PCR (EDTA tube)
- Urinary pneumococcal antigen
CSF results
CSF acellular
- Stop antimicrobials and corticosteroids and seek alternative diagnosis
CSF shows neutrophil predominance
- Continue dexamethasone (Hameln brand) 3.3 mg IV or 4 mg oral 6-hrly
- Continue antimicrobials
- if anaphylaxis to penicillin/cephalosporin, contact consultant microbiologist/ID
- if no anaphylaxis to penicillin/ cephalosporin, continue ceftriaxone 2 g by IV infusion 12-hrly. If aged >60 yr, pregnant or with impaired cellular immunity, add amoxicillin 2 g by IV infusion 4-hrly
CSF shows lymphocyte predominance
- Consider stopping antimicrobials and dexamethasone
- Consider other diagnoses (e.g. viral meningitis, tuberculous meningitis). Discuss with consultant +/- infectious disease team
Notification
- Notify cases of suspected community-acquired meningitis immediately to consultant in communicable disease control to discuss need for prevention of secondary cases
MONITORING TREATMENT
- Neurological observations, including GCS, every 15 min in severe cases initially, then at decreasing intervals as recovers
SUBSEQUENT MANAGEMENT
- If bacterial meningitis proven or probable, continue antimicrobial treatment for 7 days, then review
- if meningococci isolated, treat for 7 days, then review
- if pneumococci isolated, treat for 14 days, then review
- if other organisms isolated contact consultant microbiologist/ID
- Withdraw dexamethasone after 48 hr unless specific indication to continue (e.g. TB meningitis)
- If encephalitis is not/no longer suspected, it is not necessary to continue aciclovir until a negative HSV PCR test result has been received
DISCHARGE AND FOLLOW-UP
- Follow-up in clinic to check for hearing loss
- Refer patients with persisting neurological deficit to appropriate specialist for rehabilitation:
- aged <65 yr – rehabilitation department
- aged ≥65 yr – consultant geriatrician linked to medical firm
Last reviewed: 2023-10-23