DO NOT USE - ALL INFORMATION LIKELY INCORRECT IF NOT ACTIVELY DANGEROUS
Please use current guidelines available on the UHNM intranet for patient treatment
Please use current guidelines available on the UHNM intranet for patient treatment
PAIN
- Pain is common in patients with life-limiting illness
- Physical, psychological, social and spiritual factors can influence the experience of pain
- Pain can be well controlled in the majority of patients
Types of pain
- Visceral/soft tissue pain
- likely to be opioid sensitive
- Bone pain
- often partially opioid sensitive
- may respond to NSAIDs, radiotherapy and bisphosphonates
- Nerve pain
- partially opioid sensitive
- may respond well to adjuvant analgesics
Pain assessment
- Take a pain history using SOCRATES
- S - Site
- O - Onset
- C - Character
- R - Radiation
- A - Associated symptoms
- T - Timing
- E - Exacerbating and relieving factors
- S - Severity
- Use a pain scale
- 0-10
- visual analogue scale
- Analgesic history
- current analgesia
- previously tried analgesia
- effectiveness of treatment
- side effects of treatment
PAIN MANAGEMENT
Principles
- Identify and treat cause of pain if possible
- Select treatment appropriate for the pain and patient’s needs
- Keep it simple and use oral medication whenever possible
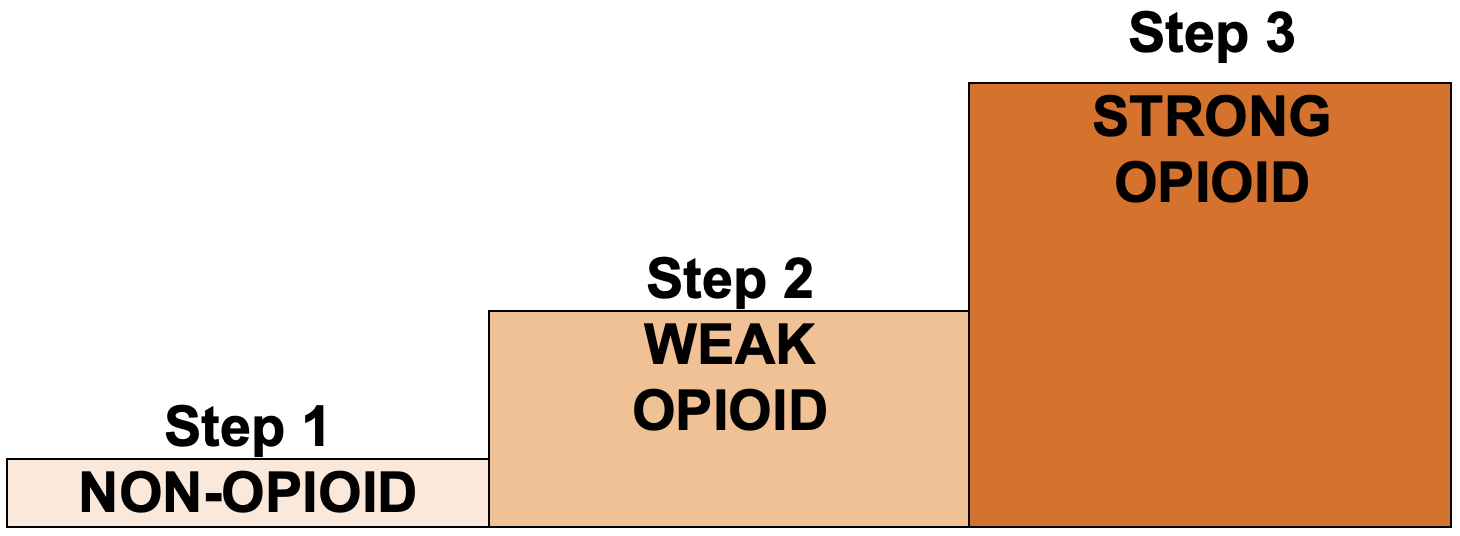
- Pain relief should be by the mouth (oral), by the clock (regular) and by the WHO analgesic ladder
- add adjuvant analgesics (e.g. NSAID/anticonvulsant/antidepressant/antispasmodic) with any step
Step 1 - non-opioid
Paracetamol
- Analgesic and antipyretic
- Dose: 500 mg–1 g 4–6 hrly (maximum dose 4 g in 24 hr)
Non-steroidal anti-inflammatories – NSAIDs
- Anti-inflammatory, anti-pyretic and analgesic
- 1st line NSAID – ibuprofen
- 1.2–2.4 g daily in 3–4 divided doses
Caution
- See BNF for cautions and contraindications before starting NSAID
- History of gastroduodenal ulceration – prescribe gastroprotective drug (e.g. PPI)
- Concomitant corticosteroids or anticoagulant or dual antiplatelet therapy – prescribe gastroprotective drug (e.g. PPI)
Step 2 – weak opioid
- Useful for moderate pain
- Seldom useful to change from one preparation to another
- If regular doses do not provide adequate analgesia, move up WHO analgesic ladder to Step 3
- Prescribe regular laxative to prevent constipation
Drugs
- Codeine 30–60 mg 4-hrly (maximum dose 240 mg in 24 hr)
- Co-codamol available as:
- 30/500 (codeine 30 mg with paracetamol 500 mg)
- dose: 2 tablets 4–6 hrly (maximum 8 in 24 hr)
Step 3 – strong opioid
- If regular weak opioid not controlling pain, initiate modified release morphine (e.g. Zomorph®, MST®)
- usual starting dose 10–15 mg oral 12-hrly
- remember 60 mg codeine 6-hrly is equivalent to 24 mg oral morphine in 24 hr
- Also prescribe as required immediate release morphine (e.g. morphine sulphate solution) for breakthrough pain
- prescribe one-sixth of the total daily dose of regular morphine (usually 2.5–5 mg)
Communication
- Ask about and discuss any concerns and misconceptions about starting strong opioids
- Provide verbal and written information on the use of strong opioids
- how to take them
- side effects
- safe storage
- how pain will be reviewed and who to contact if any problems
- If patient wishes to continue to drive, give verbal and written advice on the law on driving when taking opioid medications
Review and titration
- Nursing assessment of pain at least 4-hrly (e.g. drug rounds, observations)
- Medical review of pain control 24–48 hr after starting regular strong opioids
Patient still experiencing pain and pain is opioid sensitive
- Consider increasing regular dose
- add up total amount of morphine given in last 24 hr including modified release and immediate release morphine. Divide by 2 and prescribe 12-hrly as modified release (rounded to the nearest 5 mg)
- ensure dose of as-required immediate release morphine is adjusted when the dose of modified release morphine changed. It should be one sixth of the total daily dose of regular morphine
- see Example
Side effects
- Constipation can occur with all opioids
- prescribe regular laxatives when prescribing regular strong opioids
- it may be necessary to increase the dose of laxatives as the dose of morphine increases
- Nausea may occur when strong opioids started or dose increased but this is likely to be transient
- if nausea develops, use regular haloperidol 1.5 mg oral or SC at night
- consider stopping after 5 days
- Drowsiness or impaired concentration may occur when strong opioids started or at dose increase. If persistent or severe:
- if pain controlled, reduce dose
- if pain not controlled, consider switching to alternative opioid. See Alternative opioids below
- if side effects persist or considering alternative opioids, refer to hospital palliative care team
Alternative opioids
- May be used to improve side effect profile
- Oxycodone is the preferred second line opioid
- Do not use fentanyl patches to manage uncontrolled pain due to long half-life
- See Opioid Equivalent Tables
- use dose in equivalence table as an approximate guide
- If considering alternative opioid preparations, seek advice from hospital palliative care team
Opioids by continuous subcutaneous infusion
- Unless there is a problem with absorption or administration, opioids via continuous subcutaneous infusion will not provide better analgesia than oral route
- See Continuous subcutaneous infusion (CSCI) in palliative care guideline
Last reviewed: 2023-11-12