DO NOT USE - ALL INFORMATION LIKELY INCORRECT IF NOT ACTIVELY DANGEROUS
Please use current guidelines available on the UHNM intranet for patient treatment
Please use current guidelines available on the UHNM intranet for patient treatment
INDICATIONS
- Infusion of drugs irritant to veins
- Long-term IV feeding, antimicrobials, chemotherapy (especially tunnelled catheters)
- Persistently difficult peripheral venous access
- Insertion of Swan-Ganz catheter or intracardiac pacing device
- Use of invasive cardiac output monitoring device that requires CVC
CONTRAINDICATIONS
- Sepsis at cannulation site
- Carotid artery aneurysm (precludes use of internal jugular vein on same side)
- Coagulopathy – hypo and hypercoagulation states
CONSIDERATIONS
Danger of serious morbidity
- If not competent in procedure, organise supervision by a clinician experienced in the procedure
Sterility is essential
- Perform technique in a sterile environment where possible
- e.g. treatment room, critical care or theatre suite
- Perform procedure using full sterile technique
- Use correct equipment
- Ongoing attention to sterility of line and dressings by all users
- Removal of line when no longer required
Use of ultrasound
- Equipment and assistance to place line under 2D imaging ultrasound guidance is present in theatres and critical care
Internal jugular vein
- If in elective situation, use 2-dimensional (2D) imaging ultrasound guidance
Subclavian vein
- Consider dynamic (real-time) 2D ultrasound for subclavian vein CVC insertion
- fewer complications and a higher success rate than landmark techniques
- 2D imaging ultrasound should be available in areas where central line cannulation is carried out on a regular basis
EQUIPMENT
Before starting, be familiar with your kit
Check your central line equipment pack
Items to consider
- Sterile gloves, hat, mask, gown and full sterile drapes
- Dressing pack with gauze swabs, gallipots
- Scalpel holder with blade size 11
- Skin antiseptic. If not allergic to alcoholic chlorhexidine gluconate use 2% solution
- if allergic (but not to iodine) use alcoholic povidone-iodine solution
- Lidocaine 1% plain in a 5 mL syringe fitted with an orange (25 G) needle
- Sodium chloride 0.9% in a 20 mL syringe
- For catheters which require heparin lock, heparinised sodium chloride 10 units/mL in a 5 mL syringe
- 0 or 1 silk or nylon suture
- For peripherally inserted catheters, tourniquet
- Pressure transducer set
- Sodium chloride 0.9% (500 mL bag)
- Bionector® (Vygon) hubs for three-way taps
- prevent repeated unscrewing of ports for access to line
- if cleaned with each use, reduce infection
- Sterile clear semi-permeable occlusive dressing, or antimicrobial CVC dressing
CATHETER AND SITE
- Compare risk of infection against risk of mechanical complications
Patient-specific risks
- Pre-existing catheters
- Anatomical deformity
- Bleeding diathesis
- Some types of positive pressure ventilation
Relative risk of mechanical complications
- Bleeding
- Thrombosis
- Pneumothorax
Risk of infection
- To reduce risk of infection, consider peripherally inserted (arm) catheter
Arm vein
- Infection risk low
- Minimum length of catheter 600mm
External jugular vein
- Infection risk medium
- Minimum length of catheter 200mm
Subclavian vein
- Infection risk medium
- Minimum length of catheter 150mm
Internal jugular vein
- Infection risk high
- Minimum length of catheter 150mm
Catheter type
Long-term use
- For patients in whom long-term (>3–4 weeks) vascular access is likely, use tunnelled catheter or implantable vascular access device
Lumens
- Unless multiple ports are essential for patient management, use single-lumen catheter
Total parenteral nutrition
- Use single-lumen catheter or designate one port exclusively for this purpose
High risk of catheter-related bloodstream infection
- For adult inpatients who require short-term (1–3 weeks) central venous catheterisation, use antimicrobial impregnated central venous access device (CVAD)
- if all other aseptic precautions are instituted, further reduces infection
Chlorhexidine allergy
- Do not use chlorhexidine impregnated cannula
PROCEDURE
Consent
- Explain procedure and reassure patient
- check patient not allergic to skin antiseptic
- Obtain and record consent
Position of patient and site of insertion
- Place patient into correct position for chosen approach
- Check site of introduction
Aseptic technique
- Scrub up using full sterile technique
- don gown, gloves, hat, mask and face and eye protection
- Prepare skin with antiseptic
- Drape operative field
Local anaesthetic
- Attempt aspiration on syringe before injection to ensure needle is not intravascular
- Local anaesthetic may not be necessary in anaesthetised patients
INSERTION OF CVC
- Check fit and function of equipment
Maintain venous pressure above atmospheric
- Whichever vein used, maintain venous pressure above atmospheric by correct position or tourniquet on limb to avoid air embolism
Antecubital fossa – median (basilic) or cephalic veins
- Place patient either supine or in a semi-recumbent position, with arm abducted approximately 60°
- Distend veins by tourniquet
- Turn head to same side to compress neck veins
- Abduct arm
- Partially insert catheter then release tourniquet
- before releasing tourniquet, position proximal end of catheter below level of patient's elbow to avoid air embolus
- advance catheter to predetermined length
- Catheter passage through cephalic vein may be impeded by fascia deep to axillary vein
External jugular vein
- Place patient at 20° head down
- Vein runs from angle of mandible to behind middle of clavicle
- Choose most prominent of the right or left veins
- STOP if no vein visible or palpable
- Turn patient's head to contralateral side
- Insert catheter >200 mm length
- In 50% of patients, catheter cannot be threaded into an intrathoracic vein
- if so, try finger pressure above clavicle, depressing shoulder, or flushing catheter
- use of Seldinger or a spiral J-shaped wire may help
- DO NOT use excessive force
Internal jugular vein
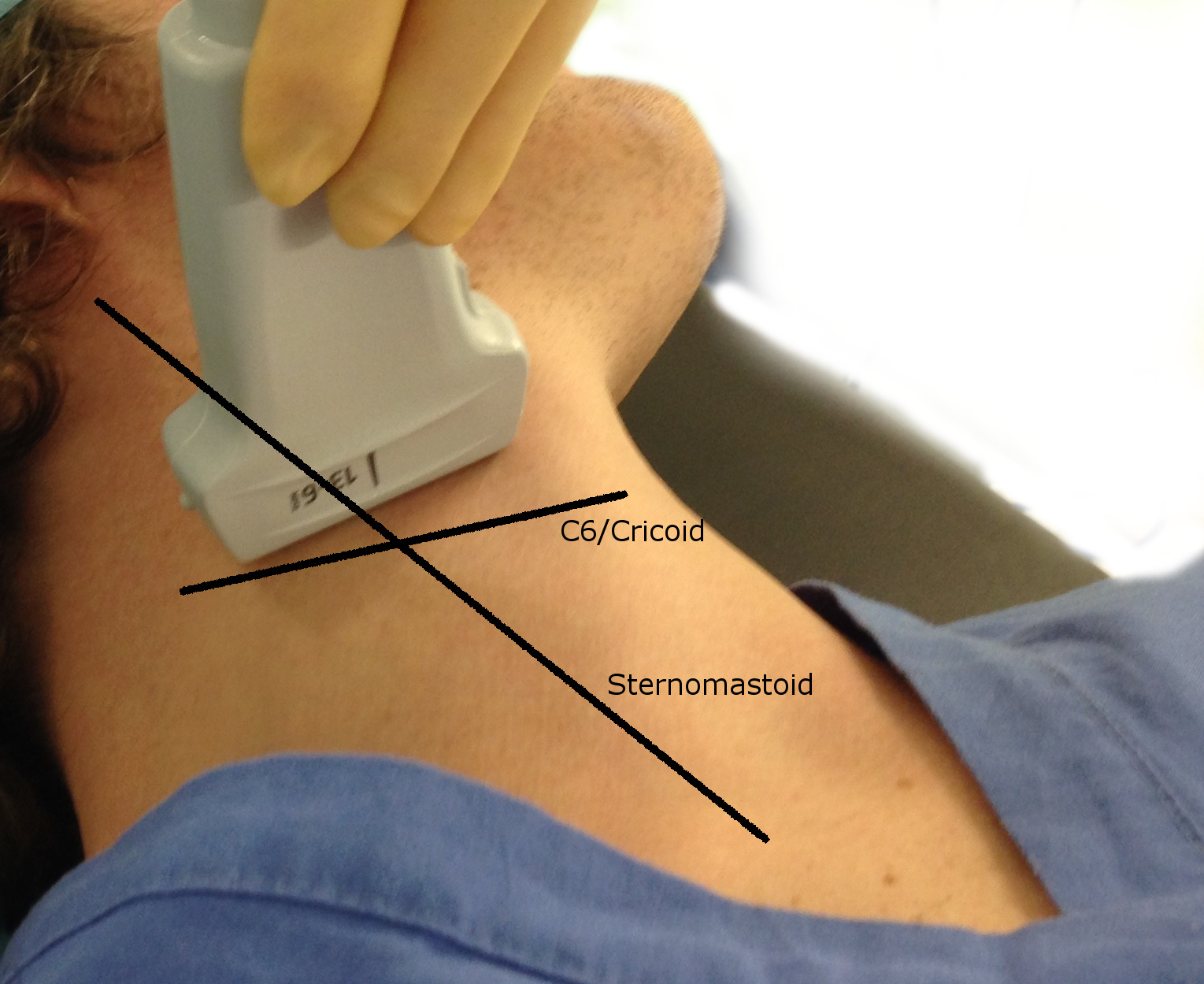
- See Figure 1
- Place patient supine, at 20° head down with head turned to contralateral side
- Preferentially use right jugular vein running behind sternomastoid close to lateral border of carotid artery
- not left to avoid injury to thoracic duct
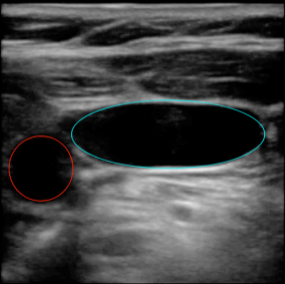
- Use 2-D imaging ultrasound guidance to identify vein and correct placement of guidewire
- see Figure 2
- Insert cannula
- operators of limited experience can try cannulation with the smaller locator needle/catheter to locate vein first and then use that as guide
- if artery is punctured, compress firmly for ≥5 min
AFTER INSERTION
- Aspirate blood on all lumens to check catheter position before injecting fluid
- On connection to pressure transducer, CVP waveform should be visible, not arterial
- Fix catheter with suture at clip site and securing holes at hub for internal jugular lines
- Cover insertion site with a clear sterile dressing
Chest X-ray
- Look for pneumothorax
- Check tip of a right-sided line is at or above the level of the carina
- confirms tip of catheter lies above pericardial reflection to avoid arrhythmias and perforation
- A left-sided line should ideally lie above the carina but:
- preferable to have the line in the SVC lying parallel to the vein (e.g. in a vertical position) rather than abutting against the wall of the SVC or lying high in the innominate vein
COMPLICATIONS
Injury to vital structure
- Pneumo- or haemothorax, arterial puncture
- Damage to thoracic duct or phrenic nerve
Arterial insertion
- Confirm by placing a small gauge cannula over guide wire and into vessel and transducing pressure before dilation
Tear of vein
- Avoid by inserting dilator no more than a few cm
Kinking of guide wire
- Avoid a perpendicular approach into vein
Air or guidewire embolus
- Place patient in head-down position during insertion of line
- If not in use ensure all ports closed and clamped
- Do not lose sight of guidewire externally at any time
Cardiac arrhythmias
- Usually stop spontaneously
- If persistent, withdraw catheter into SVC
- If severe, treat
Perforation of myocardium, mediastinum or pericardium
- Ensure free aspiration of each lumen
- Transduce main lumen and check position on X-ray
- If suspected, withdraw catheter and stop infusion
Infection, local or systemic sepsis
- Take great care with aseptic technique
AFTERCARE
Strict asepsis at all times
- Change IV giving set as per hospital protocols using aseptic technique
- Use needleless connectors where available
- if possible, do not inject drugs or take blood samples through rubber bungs
- Maintain continuous flow through catheter to prevent clotting
- if clotting occurs, try to clear by injecting 2–5 mL heparinised sodium chloride 0.9% 10 units/mL under pressure
Infection
- Monitor venepuncture site for infection daily
- If an infection occurs, see Management of central catheter-related sepsis in Artificial nutritional support in Surgical guidelines
Last reviewed: 2023-11-16