DO NOT USE - ALL INFORMATION LIKELY INCORRECT IF NOT ACTIVELY DANGEROUS
Please use current guidelines available on the UHNM intranet for patient treatment
Please use current guidelines available on the UHNM intranet for patient treatment
- Acute painful crisis in sickle cell disease (SCD) is a medical emergency
- Ensure pain relief administered within 30 min of presentation to clinical area
- Alert haematology to all admissions from outset
ACUTE COMPLICATIONS
VASO-OCCLUSIVE CRISIS (VOC)
Symptoms and signs
- Severe pain (usually in extremities, back or abdomen)
- Dehydration
- Enlarged liver or spleen
- Bone pain
- Low grade fever (<38°C) even in absence of infection
History
- Is pain similar to that of a sickle cell crisis or is it different in any way?
- Analgesia already taken for current episode?
- Any precipitating factors - infections, dehydration, stress, exercise, temperature extremes?
- Any complicating factors:
- shortness of breath/cough/chest pain?
- if YES consider ACS
- headache/neurological symptoms
- if YES undertake full neurological examination see Acute stroke and other complications
- abdominal pain/priapism
- features to indicate infection
- assess features of other non sickle related presentations
- shortness of breath/cough/chest pain?
- Previous SCD admissions and complications?
- Other medical history
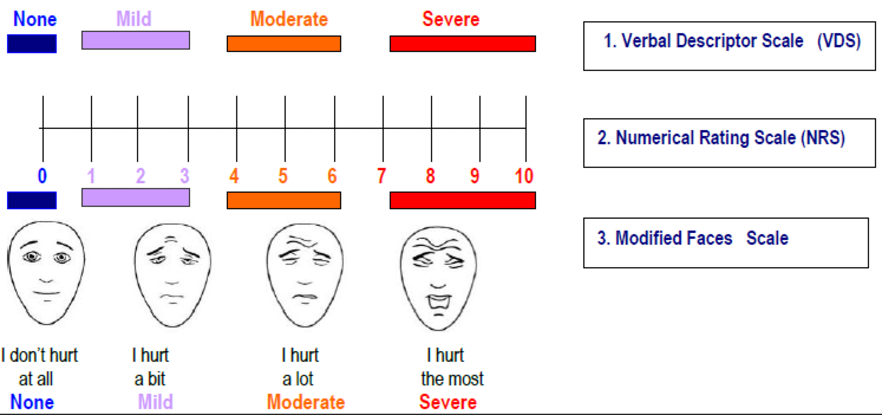
- Use age-appropriate pain score
Observations/examination
- Temperature, pulse, BP, respiratory rate and oxygen saturations on air
- Hydration status
- Enlarged liver or spleen
- If neurological symptoms/headache – full neurological findings
- fever – low grade temperature <38°C can occur in absence of infection
Investigations
- FBC and reticulocyte count
- check whether Hb and reticulocyte count similar to patient’s baseline
- reticulocytopenia may indicate virus-induced bone marrow aplasia - send parvovirus serology
- Group and screen (G&S)
- in new patients, obtain full red cell phenotype
- U&E, LFT, CRP
- If fever or relevant symptoms or signs, septic screen (including blood cultures, MSU, throat swab)
- If chest or abdominal signs - CXR
- If O2 saturations <95% or concerns re acute chest syndrome - ABG
- If new to trust - Hb electrophoresis
- If abdominal signs - CXR, abdo XR +/- USS
- If diarhoea/abdominal pain on desferrioxamine (Desferal®) chelation - screen Yersinia on blood and stool and stop desferrioxamine
- If history of trauma or unexplained swelling - consider X-ray (not indicated routinely)
IMMEDIATE TREATMENT VOC
Analgesia
- Select pain assessment tool (PAT)
- Document pain assessment score using appropriate tool
- Administer first dose of analgesia within 30 min of presentation to clinical area
- Ensure drug, dose and administration route are suitable for severity of pain and age of patient
- Refer to patient’s individual care plan if available
- Not all patients require opioid analgesia (although many do)
- Offer a bolus of strong opioid to all patients presenting with:
- severe pain
- moderate pain not relieved by analgesia already taken
Non-opioid and weak-opioid analgesia
- If no contraindications, offer all the following regularly:
- paracetamol 1 g oral 6-hrly
- if well hydrated and eGFR ≥30 mL/min, ibuprofen 400 mg oral 8-hrly or alternative NSAID
- dihydrocodeine 30-60 mg oral 4-6 hrly (maximum 240 mg/24 hr) or tramadol 50-100 mg 6-hrly (maximum 400 mg/24 hr)
- Review doses in presence of renal impairment
Opioid analgesia for severe pain
- Opiate naïve with weight ≤50 kg; morphine 2.5-5 mg SC/oral usually 2-4 hrly
- Opiate naïve with weight >50 kg; morphine 5-10 mg SC/oral usually 2-4 hrly
- Non-opiate naïve; morphine 5-10 mg SC/oral usually 2-4 hrly
- Do not use pethidine for treating pain in an acute sickle cell episode (associated with seizures, muscle abscesses and contractures). Named patient basis only
- Avoid IV morphine to limit need for canulation and preserve (often difficult) venous access. SC morphine is just as efficacious as IV for most patients
- if IV morphine indicated on individual patient plan - give morphine 0.1-0.15 mg/kg IV (maximum 10 mg) over 5 min up to every 2 hr
- Consider patient controlled analgesia (PCA) once initial pain under control
Auxiliary medications
- Ensure regular laxatives prescribed
- Prescribe antiemetics e.g. ondansetron 8 mg 12-hrly
- Prescribe PRN antipruritic medication e.g. loratadine 10 mg once daily
Monitoring
- Assess analgesia effectiveness 30 min after administration
- consider repeating/increasing dosage according to efficacy
- 30 min and 1 hr after analgesia, monitor;
- full observations
- sedation score
- pain score
- Assess pain every 30 min until satisfactory pain relief achieved, then monitor at least every 4 hr (use pain score)
- Monitor patient observations 4-hrly; or more frequently if clinical concerns
- If respiratory rate <8 per min, patient unrousable or cyanosed - manage as opioid-induced respiratory depression
- stop all opiods
- call for urgent medical assistance
- administer naloxone 80 microgram IV as slow IV bolus. Further doses may be required. See Naloxone guideline in surgical guidelines and call emergency response team
Fluid replacement
- Encourage oral fluids 2-3 L/day
- IV fluids should only be used if patient is dehydrated or unable to drink
- Ensure accurate fluid balance chart maintained
- Do not canulate veins in ankles/feet as high risk of leg ulceration
- If unable to give orally, give glucose (4%) and sodium chloride (0.18%) 1 L by IV infusion over
3 hr; - then follow IV fluid maintenance guideline
Oxygen therapy
- Of doubtful use if patient is not hypoxic
- Monitor pulse oximetry with regular readings on air and on oxygen (if in use)
- If O2 <95% on air;
- urgent medical review - ?acute chest syndrome ?opiate-induced respiratory suppression ?infection/PE/other
- start oxygen 2-4 L/min by mask/nasal canulae - see Hypoxaemia guideline
- if O2 <95% on air, check ABG
- increase frequency of observations
- If SpO2 cannot be maintained >94%, discuss with haematology team and critical care team
Blood transfusion (see transfusion section or regional guidelines for further details)
- Not indicated in uncomplicated painful crisis
- No evidence it shortens duration of crisis
- Baseline Hb often 60-90 g/L in HbSS patients. Transfusion may cause harm through hyperviscosity
- Do not exceed 10-20 g/L above baseline (or baseline if steady state >100g/L) especially if HbS >30%
- Discuss with haematology team before any transfusion
- Ensure special blood requirements met (extended phenotype matched, HbS negative)
- link closely with transfusion laboratory
Antimicrobials
- If temperature >38°C undertake septic screen and start sepsis pathway
- focus antibiotics to likely source of infection - see trust guidelines
- If no active infection, continue prophylactic antimicrobials (if routinely taking)
Infection control alerts
- Check IC alert
- If IC alert not available, check previous 12 months of microbiology reports
- If MRSA present, treat as tagged for MRSA. See MRSA management guideline
- if ESBL, MGNB, CARB present, treat as tagged for ESBL. See ESBL/MGNB/CARB management guideline
Thromboprophylaxis
- Unless contraindicated, give thromboprophylaxis
- see VTE prophylaxis guideline
Supportive treatment
- Offer incentive spirometry
- Folic acid 5 mg once daily
- Ensure antiemetics/laxatives prescribed
Ongoing Management
- Monitor patients closely
- to determine the effectiveness of analgesia, using a pain-scoring tool
- assess vital signs including sedation score for adverse effects of analgesia
- Use incentive spirometry to reduce basal atelectasis
- Haematology team may discuss patients with difficult pain management with specialist haemoglobinopathy team (Sandwell and West Birmingham Hospitals) or acute pain team
- no role for palliative care input
Discharge following VOC and follow-up
- Discharge home when pain controlled by oral medication
- Provide 3-4 days' supply of analgesia
- Schedule timely follow-up review in red cell clinic
- Before leaving hospital ensure information given (NICE quality standard 2014) on how to:
- access specialist support
- get extra medication
- manage any side effects of treatment
- See intranet > haematology > Patient information leaflets > SCD Care following discharge
ACUTE CHEST SYNDROME (ACS)
- Acute life-threatening complication of SCD
- Characterised by breathlessness, hypoxia, fever and new onset pulmonary infiltrates in CXR
- leading cause of premature mortality in SCD
- third most common cause of death in adults
- mortality 3% even with optimal care
- Early recognition and prompt escalation with specialist support is essential
- Discuss urgently with haematologist
- Have low threshold for involvement by local critical care outreach services
Clinical presentation
- In 50% cases preceded by 24-72 hr history of more typical VOC
- increased risk in postpartum and post-operative periods
- Patients may appear well compensated initially, followed by rapid deterioration - have low threshold for escalation
- Symptoms include:
- chest pain - especially sternal or rib pain
- shortness of breath
- increasing oxygen requirement
- fever
- On examination
- hypoxia
- tachycardia
- dullness to percussion
- crackles, bronchial breathing, wheeze or reduced air entry
- Hypoxia is a particularly important sign
- Closely monitor and rapidly escalate patients if:
- fall in SaO2 of 3% from baseline, or
- SaO2 <95% on air
- consider other contributors to hypoventilation e.g. inadequate pain relief, opioid induced narcosis
Investigations
- If SpO2 <95% on room air, ABG
- Room air ABG unless
- patient in obvious respiratory distress
- if oxygen stopped briefly and SpO2 saturations fall to <85%
- FBC and reticulocytes - fall in baseline Hb of >10 g/L or a fall in platelets predict morbidity
- Renal function, liver function and CRP
- G&S: inform blood bank that patient has sickle cell anaemia to allow appropriate products to be requested
- CXR - note changes may lag behind clinical picture. Bilateral infiltrates are typical of ACS
- Sputum for MC&S
- Respiratory viral PCR (either swab or nasopharyngeal aspirates as per local protocols)
- Atypical serology (on presentation and repeated at 3 weeks)
- Urinary legionella and pneumococcal antigen
- Blood cultures in febrile patients
Potential precipitants and differential diagnosis
- Respiratory infections
- identifiable as a precipitant in 38% of cases
- Pulmonary embolism
- can co-exist or precipitate chest crisis
- history is usually of more sudden onset
- patient recognises pain as not typical of sickle cell
- D-dimer is invariably raised
- consider CTPA or VQ if there is clinical suspicion of PE
- Patients with pre-existing respiratory disease
- patient with asthma at increased risk of ACS
- Fluid overload in at risk populations
- consider if cardiac disease, renal impairment, transfusion associated fluid overload (TACO)
Severity assessment
- Increased morbidity seen with following features:
- increasing oxygen requirement
- increasing respiratory rate
- decreasing platelet count
- fall in Hb from baseline of 10 g/L
- neurological symptoms
- multi-lobar involvement on CXR
Management
- Contact on-call haematologist early in any patient suspected of ACS
- Regular observations
- to include pulse rate, blood pressure, respiratory rate and pulse oximetry
- at least 4-hrly or as per EWS
- more frequently if on PCA or clinical concerns
- Analgesia as per VOC guidance
- IV crystalloid until patient able to maintain hydration orally
- monitor fluid balance every 24 hr
- Give parenteral antibiotics to all patients with ACS
- refer to local microbiology protocols for severe community acquired pneumonia
- ensure atypical organisms are covered
- Physiotherapy
- refer all patients for same day evaluation by chest physiotherapist
- offer all patients incentive spirometry to aid lung expansion
- Thromboprophylaxis with low molecular weight heparin
- unless absolute contraindication
- Transfusion - may be life-saving
- involve haematology specialist from outset
- if at risk of further deterioration - initiate transfusion early
- consider early top-up in hypoxic patients with severe anaemia (Hb<70g/L) to prevent futher deterioration
- If deteriorating patient or Hb >90 g/L, exchange transfusion - discuss with haemoglobinopathy co-ordinating centre to arrange
- undertake in HDU setting
FEVER AND SEPSIS IN SCD
- Patients with SCD are at increased risk of severe infections due to functional asplenia
- sources of infection are chest, urine, osteomyelitis, indwelling central venous access devices (CVAD) and hepatobiliary
- Complete sepsis 6 - See Sepsis guideline
- Low grade temperature <38°C can occur with vaso-occlusive crisis in the absence of infection
- If temperature ≥38°C and/or suspected sepsis ensure
- full clinical review
- septic screen: cultures of blood, urine, and any other potential sites of infection
- CXR
- if there is a history of travel to an endemic region, malaria screen
- Antibiotics as per local antibiotic guideline
- if source unknown - broad-spectrum antibiotics to include coverage for pneumococcus and gram negative organisms, including Salmonella
- if blood cultures become positive admit for parenteral antibiotics
- If well with isolated temperature rise consider outpatient management
- Admit to hospital if:
- acute painful crisis (severe that cannot be managed with home analgesia)
- suspected ACS (chest pain, breathlessness/increasing oxygen requirements, pulmonary infiltrates on CXR)
- dehydration, vomiting
- requirement for supportive care, e.g. IV fluid or oxygen
- unreliable compliance/support
- consider if indwelling catheter
OSTEOMYELITIS
- Clinical presentation similar to vaso-occlusion
- pain, localised tenderness, warmth, swelling, fever and leucocytosis
- note bone pain more likely VOC than osteomyelitis
- Increased incidence in SCD from infection of infarcted bone
- Usually due to salmonella (especially non-typical serotypes such as Salmonella typhimurium, Salmonella enteritidis), followed by Staphylococcus aureus and gram-negative enteric bacilli
- If pain persists beyond typical VOC, or pain is atypical and fever continues, investigate:
- blood cultures
- bone biopsy/aspiration in selected cases - positive result confirms diagnosis
- imaging - plain X-rays and MRI are not sufficiently discriminating to differentiate
- Discuss management with haematologist and orthopaedic surgeon
- broad spectrum antibiotics to cover salmonella and staphylococcus pending culture results
- if organism isolated, tailor choice of antibiotic
- continue antibiotics for 6 weeks
- drainage for fluid accumulation that does not respond to antibiotics
- broad spectrum antibiotics to cover salmonella and staphylococcus pending culture results
ACUTE ANAEMIA
- Patients with SCD have a variable degree of anaemia
- due to ongoing intravascular and extravascular haemolysis
- tolerate anaemia well in the steady state
- may become symptomatic of anaemia if rapid, significant fall in Hb - usually of at least 20 g/L
- Worsening anaemia may develop due to:
- increased haemolysis e.g. infection, VOC, G6PD deficiency, transfusion reaction
- reduced erythropoiesis e.g. parvovirus infection, medications
- blood loss e.g. bleeding
- sequestration of blood e.g. spleen sequestration (commoner in milder phenotypes), liver sequestration
- May be multiple co-existing causes for acute anaemia
- Take into account history of bleeding, infection, travel, malaria risk, medications e.g. hydroxycarbamide, organomegaly, transfusion
- Investigations to include:
- reticulocyte count
- LFTs including unconjugated bilirubin
- direct Combs test (DCT)
- G6PD assay (in steady state)
- malaria screen (if relevant travel history)
- parvovirus serology (?positive IgM)
- infection screen
- clinical examination for rapidly enlarging painful splenomegaly/hepatomegaly
ACUTE STROKE AND OTHER CNS COMPLICATIONS
- Adults with SCD at risk of both acute ischaemic and haemorrhagic stroke
- risk of acute ischaemic stroke increasing with older age
- Acute presentations can include:
- headache
- seizures
- focal neurological signs
- visual impairment
- altered consciousness
- acute deterioration in cognition
- Emergency neuroimaging required in adults presenting with symptoms of transient ischaemic attack (TIA) or stroke
- Urgent review by neurologist and haematologist
- manage in hyperacute stroke unit with access to multidisciplinary support from a haemoglobinopathy specialist centre, vascular interventional neuroradiology, neurology and neurosurgery
- urgent red cell exchange recommended for patients with a sickle related acute ischaemic stroke - target HbS <30%
- in older patients with risk factors for non-sickle stroke, discuss requirement for thrombolysis with multidisciplinary team (including haemoglobinopathy coordinating centre)
- consider other causes of stroke seen in young adults without SCD - e.g. thrombophilia, CNS infection, illicit drug use, arterial dissection, congenital heart disease
- Headache - common symptom and in most cases do not indicate significant CNS pathology
- consider possibility of intracranial haemorrhage, central venous thrombosis, CNS infection and ischaemic stroke
PRIAPISM IN SCD
- Painful and prolonged (>4 hr) penile erection unrelated to sexual stimulus
- This is an emergency - urgent urological and haematological input required
- can impact significantly on erectile and sexual function
- delayed therapy of acute priapism can lead to impotence
- Lifetime incidence of priapism high
- majority of cases first episode occurs before aged 20 yr
- Stuttering priapism
- short episodes (<4 hr) of recurrent or intermittent ischaemic priapism
- self-limiting but can lead to a more sustained or fulminant episode
- Fulminant priapism
- acute ischaemic event requiring emergency treatment
- early recognition and initiation of treatment may achieve detumescence
- Assess:
- duration of episode
- presence of pain
- previous priapism and treatment
- any trauma
- medications including analgesia
- recreational drugs
- other complication of SCD
- Initial management includes:
- exercise e.g. going up and down stairs
- adequate pain relief
- hydration
- encourage to empty bladder
- offer etilefrine if available (alpha adrenergic agent)
- Early urgent urological review for consideration of surgical intervention
- penile aspiration of stagnant blood under anaesthesia to decompress the corpora carvenosum potentially followed by shunt procedure
- aim is to relieve penile ischaemia and to preserve erectile function
- results are however variable
- Transfusion
- no evidence for efficacy
- consider before surgery
ACUTE HEPATOBILIARY COMPLICATIONS OF SCD
- May be due to:
- vaso-oclusion
- gall stone complications
- infection
- unrelated diseases
- Manage in partnership with haematology, gastroenterologists, upper GI surgeons and microbiologists with experience of SCD
- Imaging to include:
- ultrasound - to look for gallstones in the gallbladder and/or common bile duct
- magnetic resonance cholangiopancreatography (MRCP) - if ultrasound has not detected common bile duct stones but bile duct dilated and/or liver tests abnormal
Gallstones
- Common in SCD
- Complications may develop due to:
- infection and inflammation of the gall bladder and biliary duct (acute cholecystitis, gallbladder empyema, ascending cholangitis)
- obstruction of biliary ducts
- acute pancreatitis
- Management to include:
- early antibiotics in view of infection risks - broad spectrum including cover for salmonella species and anaerobic organisms
- if symptomatic (occurs in 20%) refer for laparoscopic cholecystectomy
- if common bile duct stones refer for bile duct clearance (ERCP) then laparoscopic cholecystectomy
- elective cholecystectomy appropriate after acute complications settle - more urgent treatment indicated in some instance
- preferentially use laparoscopic route as fewer postoperative complications and shorter length of stay
- if asymptomatic, inform of gallstone complications and manage as per general population
Jaundice
- Present in patients with SCD - baseline degree individual to patient
- Elevation in baseline bilirubin can occur with:
- haemolysis - often exacerbated in VOC
- consider delayed transfusion reaction and hyperhaemolysis
- obstructive causes such as gallstones, biliary sludge
- intrahepatic cholestasis
- Intrahepatic cholestasis is an uncommon but severe form of sickle hepatopathy due to intrasinusoidal sickling and intracanalicular cholestasis
- Acute presentation can include:
- severe right upper quadrant pain
- acute hepatomegaly
- coagulopathy
- extreme hyperbilirubinemia (mainly conjugated) but moderately elevated liver enzymes
- Some patients can progress to acute hepatic failure
- Exclude other causes of liver dysfunction through USS/Magnetic Resonance Cholangiopancreatography (MRCP) imaging
- Biopsy is relatively contraindicated in acute hepatopathy in SCD due to the risk of bleeding and other complications
- Early exchange transfusion can improve outcome and reduce mortality
ACUTE RENAL FAILURE (ARF)
- ARF can be precipitated by:
- dehydration
- sepsis
- drugs e.g. NSAIDs, intravenous contrast
- in the context of multi-organ failure
- on the background of chronic renal failure (either from sickle related nephropathy or other aetiologies)
- ARF may be due to
- pre-renal aetiologies (e.g. dehydration)
- intrinsic renal pathology
- or post renal causes
- Management of ARF
- follow similar principles as in other patient groups
- careful fluid balance and close monitoring of renal function in all patients
- jointly with renal physician
- Haematuria
- consider renal papillary necrosis (vaso-occlusion of vasa- recta)
- may cause clot colic
- offer conservative management - hydration
BLOOD TRANSFUSION
General principles
- All patients should carry a transfusion card with details:
- ABO group, extended red cell phenotype, Rh phenotype and
- existence of any red cell alloantibodies (current and historic)
- Transfusion history is important, particularly if care is a different hospital
- liase with transfusion laboratory at primary hospital to obtain transfusion history
- Advise transfusion laboratory/blood bank that transfusion is for a patient with SCD
- Discuss with haematology to determine if simple top-up or exchange transfusion needed
- Determine post-transfusion target Hb and HbSS
- Record and document transfusion triggers and indications
- Monitor closely both during and after completion of transfusion for:
- immune haemolytic transfusion reaction (IHTR)
- delayed haemolytic transfusion reaction (DHTR) and
- hyper haemolysis
- All patients to have annual viral screening for Hepatitis B, C and HIV 1 and 2
Venous access
- Simple top-up transfusion: single peripheral venous cannula
- Manual exchange transfusion: 2 separate large bore venous access
- one for transfusion and inlet port (wide bore needle grey/orange) and
- another for venesection (vascath: femoral/central neck line)
- Automated red cell exchange: femoral line/vascath - double lumen
- Long-term transfusion programme: consider port-a-cath
Top-up transfusion
Indications
- Severe anaemia (Hb <50 g/L) owing to:
- hepatic or splenic sequestration
- red cell aplasia or haemolysis
- Severe anaemia when decrease in Hb >20% from baseline in a symptomatic patient (heart failure, dyspnoea, hypotension and marked fatigue)
- Transfuse to baseline Hb (patient’s Hb in steady state)
- Consider when exchange transfusion indicated and starting Hb <50 g/L
- Discuss with haematologist
Exchange transfusion
Indications
- Severe chest syndrome
- New ischaemic stroke
- Multi-organ failure
- Consider in priapism
- Do not initiate exchange transfusion before discussing with haematologist
Targets
- To reduce HbS to <30%
- To maintain Hb <100 g/L
- note: haematocrit of donor blood is approximately double that of patient
- To maintain steady blood volume throughout procedure
Venous access
- Ideally, identify 2 ports for venous access; 1 for venesection, the other for transfusion
- in emergency, consider a central line, or arterial line (e.g. on ITU)
- Exchange transfusion is performed isovolaemically (equal quantities in and out)
- Ensure patient well hydrated before exchange
- prehydrate with sodium chloride 0.9% 500 mL if Hb >80 g/L
Method
- Procedure and regimen will depend on investigations and must be discussed with haematologist
HYDROXYCARBAMIDE
- Licenced for use in SCD
- Commenced by dedicated red cell team
- Continue hydroxycarbamide during admissions unless cytopenia (see below) or toxicity suspected
- Reduces frequency of VOC, ACS, need for blood transfusion, hospitalisation and mortality in adults with SCD
- Works by increasing Hb F levels, reducing surface expression of adhesion molecules, reducing bone marrow production of neutrophils and reticulocytes, improving red cell rheology, and improving nitric oxide availability
- Indicated in adult patients if:
- SS/Sβ 0 with ≥3 moderate to severe pain crises in a 12 month period
- SS/Sβ 0 who have a history of severe and/or recurrent ACS
- SS/Sβ 0 who have sickle associated pain or severe symptomatic anaemia that interferes with quality of life or activities of daily living
- consider in SCD with genotypes other than SS/Sβ 0 who have recurrent acute pain, acute chest syndrome or episodes of hospitalisation; or for other indications on a case-by-case basis
- Contraindicated in pregnancy
- Dose dictated by weight, clinical response, blood test monitoring
- Side effects include cytopenia, hyperpigmentation of nails/skin, GI toxicity including diarrhoea and constipation, nausea and vomiting, skin rash, alopecia, oral ulcers, azoospermia/oligospermia
- Offer male patients sperm cryopreservation before commencing treatment
- Prescribed by secondary care (unless formulary agreement with primary locally)
- Monitoring bloods 8-12 weekly bloods once dose established, to include FBC, reticulocytes, U&E, LFT
- Stop hydroxycarbamide if any of the following apply:
- neutrophils <1.0 x 109/L
- platelets <80 x 109/L
- reticulocytes <1%
- Hb 30 g/L below baseline
- Hb >120 g/L or rise >30 g/L above baseline
- Link with red cell team regarding recommencement (with dose reduction)
Last reviewed: 2024-07-17