DO NOT USE - ALL INFORMATION LIKELY INCORRECT IF NOT ACTIVELY DANGEROUS
Please use current guidelines available on the UHNM intranet for patient treatment
Please use current guidelines available on the UHNM intranet for patient treatment
RECOGNITION
- Vitamin deficiency usually develops slowly over several months to years
- Vitamin deficiency signs and symptoms may be subtle at first
- increase as the deficiency worsens
Symptoms
Neurological
- Numbness or paraesthesia
- Muscle weakness
- Unsteady movements
Megaloblastic anaemia
- Breathlessness
- Fatigue
- Dizziness
Non-specific
- Memory loss
- Personality changes
- Mental confusion or forgetfulness
- Irregular heartbeats
Signs
- Pale or yellowish skin
- Glossitis
- Peripheral neuropathy
- especially proprioception
- Sub-acute combined degeneration of the cord
- which may occur in the absence of anaemia
Assessment
- Diet
- Features of malabsorption
- Personal/FH of autoimmune conditions
- GI surgery
- Medication use
- e.g. proton pump inhibitors, metformin, OCP
- Pregnancy and OCP
- oestrogen reduces serum B12 (but not functional B12)
- by 25% on oral contraceptive pill
- by <30% by third trimester of pregnancy
- level >150 pg/mL may therefore be normal
Investigations
- FBC
- Folate
- Serum cobalamin (B12)
- Anti-intrinsic factor Ab (anti-IF Ab)
- if suspect PA, test for anti-IFAB regardless of cobalamin levels
INITIAL MANAGEMENT
Pancytopenia
Refer to haematology
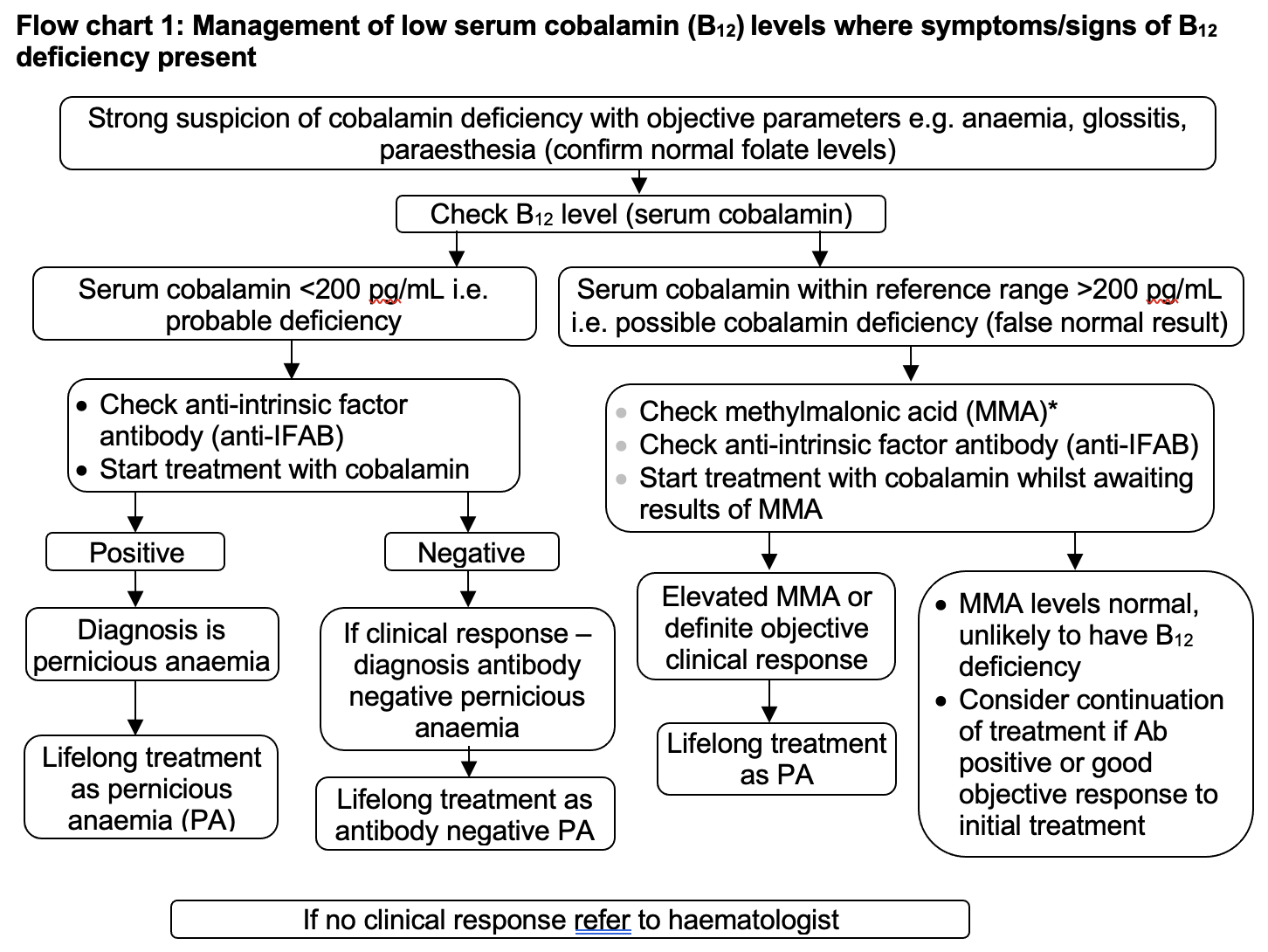
Symptoms/signs of B12 deficiency present
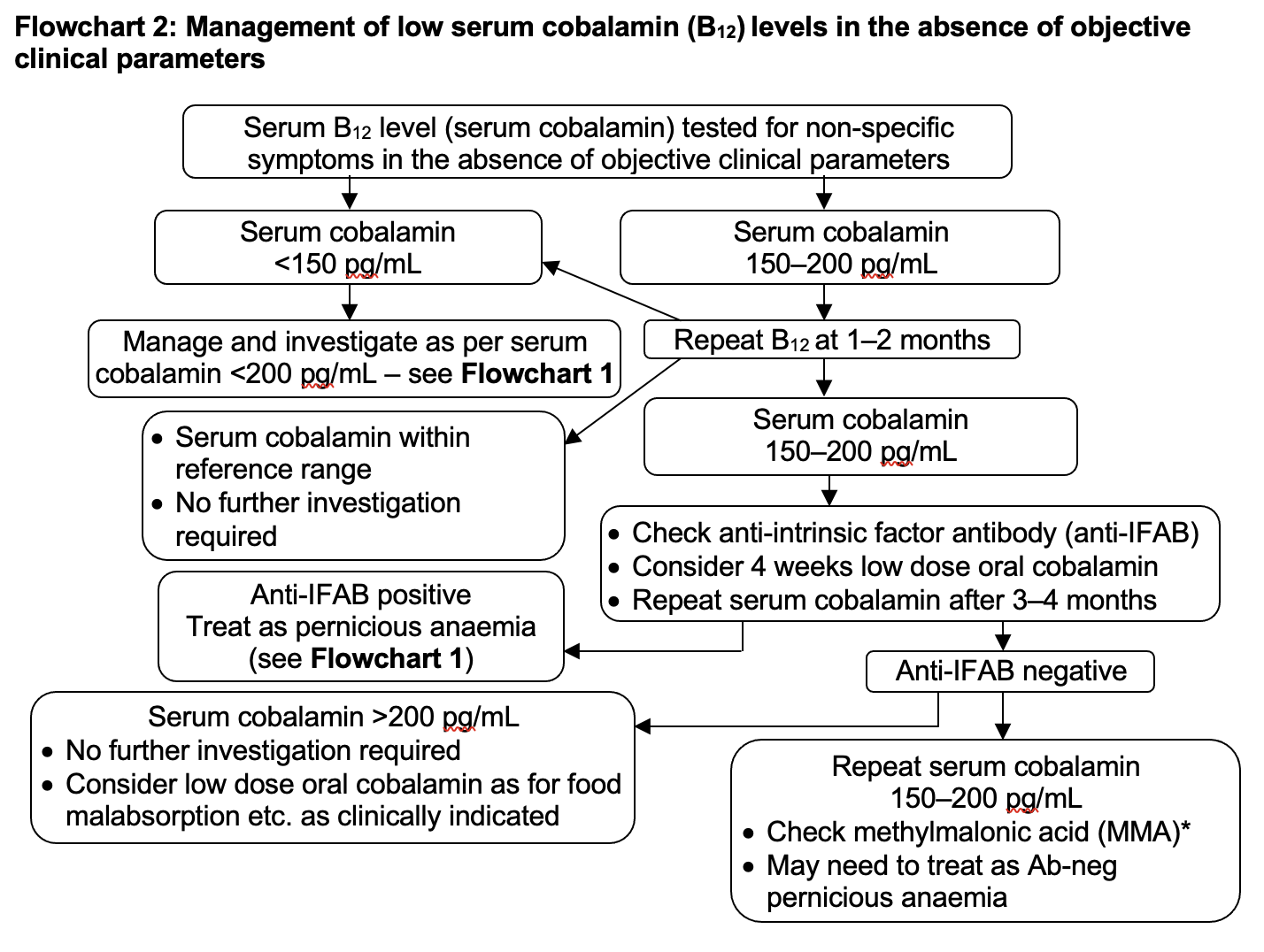
B12 low but symptoms/signs absent
- B12 ≤200 pg/mL
- Non-specific symptoms
TREATMENT
Pernicious anaemia
- Prescribe vitamin B12 as hydroxocobalamin
- Treatment regimens are dependent on symptoms/signs. See BNF
Dietary cause
- Dietary sources of B12 include eggs, milk/dairy products, salmon, fortified products e.g. cereals
- In the absence of neuropathy, consider oral cyanocobalamin 50-150 microgram daily taken between meals (although higher doses may be required)
- check B12 levels at 1-3 months
- Duration of B12 supplementation depends on the cause of the deficiency and response
- When using oral cyanocobalamin, caution regarding possible emerging PA
RBC transfusion in chronic anaemia
- If severe symptoms of anaemia, discuss with haematology before initiating transfusion which is rarely required
ASSESSING RESPONSE
- If patient receiving IM hydroxocobalamin, do not routinely check B12 levels
- Monitor for hypokalaemia after commencing B12 replacement and consider replacement
- If PA, assess reticulocyte response at 7-10 days
- suboptimal response may indicate concomitant iron deficiency
DISCHARGE
- Inform GP of:
- cause
- treatment
- monitoring required
Last reviewed: 2024-01-10